Caregiver: "Why Is This Person Coughing Whenever I Feed Them?"
 |
| Souce: Daily Caring |
What a serious question! It is a common question all caregivers ask themselves if they are directly feeding a loved one or a resident at their facility.
Imagine this, you are sitting with your mother with Dementia, a son with a developmental disability, or a resident with dysphagia after a stroke. Just getting them to the table where you have their food set up was a tiring chore. Then, you dip your spoon into their appropriate food texture and give them a bite.
All of the sudden, they cough once. Then twice. You wait until they say something again, like, "What is this?" You say it's peas and carrots. "No, I don't like peas and carrots". "Well, do you want your mashed potatoes instead?" They agree and you give them a bite of that. A few minutes later, they began coughing again, but this time they cough so much their face turns red. Your heart sank and you begin thinking about your setup.
"Did I give them too big of a bite?"
"Crap, if they cannot handle this, then what? Should they just not eat and have a G-Tube?"
"I was watching them, why is this happening??"
"I saw them swallow! I'm doing everything the therapist told me to do. Why are they coughing???"
It is tough watching someone you care for suffer with something as basic as swallowing. Eating is considered a basic activity of daily living, so when that ability becomes impaired, it can be devastating.
:max_bytes(150000):strip_icc():format(webp)/problems-swallowing-dysphagia-and-multiple-sclerosis-2440815-V2_A-01-33a5bbe6aea1407c991c2f3d8c7db7c8.png) |
| Source: verywellhealth |
- Loss or change in appetite
- Coughing during or after eating/drinking
- Face reddens or blanches during or after eating
- Gasping for breath
- Producing a gargly or raspy voice, like they need to clear their throat
- Reflux or vomiting
 |
| Source: Anatomy Drawing Diagram |
Knowing the problem is half the battle. Now what can we do to prevent them from aspirating? What can we do to help them stop coughing?
 |
| Source: Pocket Dentistry |
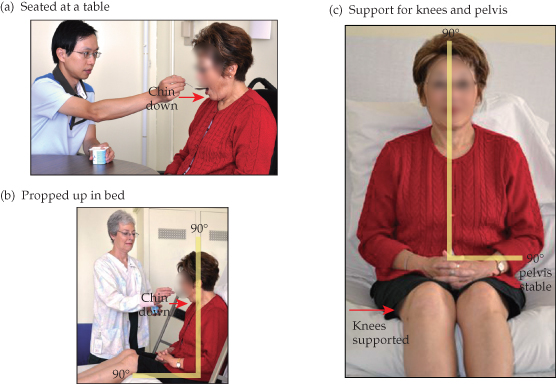
First, look at their posture; the way they sit is important. Normal alignment makes it easier for food to go down the esophagus and into the stomach 2. If they lean to much on one side or another, then it may change the pressure inside that person's gastrointestinal system (GI system) and make it easier for the stomach contents to move back up the esophagus and now towards the small intestines. Normal alignment typically means sitting upright, with knees bent, and chin is perpendicular to the floor (down when eating/drinking). Sometimes, adding postural straps, harnesses, or a different seat makes a huge difference on someone's posture and improves their ability to swallow.
Second, we must look at how we are giving the food. The standard compensatory feeding methods therapists teach caregivers are:
- Giving smaller bites of food
- Alternate bites of food with sips of liquids, especially if the food texture is dry
- Asking the person to do two swallows for every bite of food/sip of liquid (i.e. double swallow)
- Slower pace of feeding (sometimes as slow as one bite ever 10-15 sec)
- Checking the food texture or liquid consistency
- Reduce the amount of socializing so the person eating are less likely to talk and swallow at the same time.
- Modifying the environment to be quieter with less distractions
- Plan ahead. Be realistic about how much time someone needs to eat. If they take an hour to eat, then plan your day to allow them to have an hour to eat. If you have multiple people to feed, consider saving the longest feed for last.
- Use different adaptive dining equipment (if you work at a facility, ask the therapist about different equipment). Use a teaspoon instead of a regular spoon. If they always spill their drink, consider a cup with a small cut-out so the cup can tilt up more without pressing against the nose, or a smaller cup.
- Make sure to look at the resident while they eat. Do you still see food particles inside their mouth after they swallow? Ask them to swallow again before you give them another bite of food. Did they swallow but they Adam apple didn't moved? Food may still be at the back of their throat, so ask them to swallow again.
- Talk to others about your problem. If you are at home with your loved one, seek out a speech or occupational therapist to help work out specific problems, or see if they qualify for additional speech or occupational therapy to improve their swallowing abilities. If you are at a facility, speak up about the difficulties with feeding the residents and ask the team to work together on how to address larger problems. Can more time be allotted for feeding? Can more help be provided? If someone needs a quiet area to focus on eating, can they eat in the room instead?
 |
| Source: Diversified Health Partners, LLC |
1. Kendall R. L. A. K. Dysphagia Assessment and Treatment Planning: A Team Approach, 2nd Edition. Plural Publishing Inc.
2. Beckman Oral Motor Protocol. I highly recommend this course to those who want to learn more!


